In the NICU - Medical Care
Medical equipment
Neonatal units are full of equipment that you may not have seen before. This equipment helps us to look after your baby safely.
This section provides a brief description of some of the equipment you may see around your baby in the neonatal unit.
This is a sensor that is attached to baby’s tummy to detect that they are breathing. If baby stops breathing for more than 20 seconds, this monitor will alarm.
Blood pressure is the pressure made by the heart to push baby’s blood around their body. The team looking after your baby can check blood pressure using a cuff on baby’s arm or leg, or a line in their bellybutton or their wrist or ankle. If blood pressure is low, sometimes medications are used to help keep it at a normal level.
This mattress is filled with water that can change temperature to change baby’s temperature. This is used as part of therapeutic hypothermia.
This tube is put into baby’s windpipe, usually through their mouth. It is used to give medication or breathing support directly into baby’s lungs.
A small machine that measures the level of glucose (sugar) in the blood.
 An incubator is a specially designed cot with a clear plastic cover, used for babies who are preterm or unwell. An incubator keeps a baby warm. For very small or preterm babies we can make the incubator humid to keep baby’s skin moist, which keeps baby warm and lets their skin mature slowly. Because incubators are clear, the team looking after baby can see baby and look at them very carefully. The doors on the incubator let us take care of baby while keeping them warm. See section ‘Neonatal care’ LINK.
An incubator is a specially designed cot with a clear plastic cover, used for babies who are preterm or unwell. An incubator keeps a baby warm. For very small or preterm babies we can make the incubator humid to keep baby’s skin moist, which keeps baby warm and lets their skin mature slowly. Because incubators are clear, the team looking after baby can see baby and look at them very carefully. The doors on the incubator let us take care of baby while keeping them warm. See section ‘Neonatal care’ LINK.
This pump is used to put fluids, feeds and medication into baby by an IV cannula or a feeding tube. Some pumps use syringes and some pumps can measure fluid from a bag.
IV means intravenous, which means into a vein. An IV line is a very fine plastic tube put into one of baby’s veins, in the arm, leg or scalp. IV lines are only just under the surface of the skin. Babies can be given fluids, nutrition, or medication through IV lines. Fluids given via an IV line can be referred to as IV fluids or a ‘drip’. Nutrition given through an IV line is called Parenteral Nutrition (PN). See ‘Parenteral Nutrition’ LINK.
Peripherally inserted central catheter: This is a long IV line that goes into a vein in the arm, leg or less commonly in the scalp, and the end of the line is close to the heart. These can be used for nutrition or medication. They can last for much longer than a normal IV line but must be kept very clean to prevent infection.
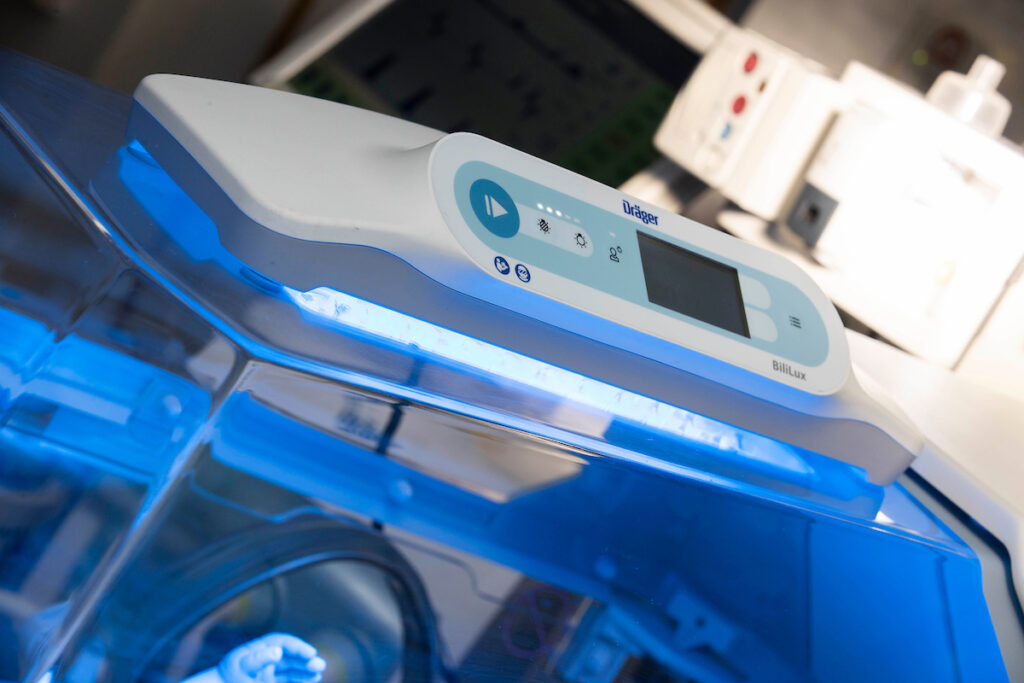 These are special lights that are used to treat jaundice, see ‘Phototherapy’.
These are special lights that are used to treat jaundice, see ‘Phototherapy’.

This measures the amount of oxygen in baby’s blood using a sensor with a red light. These are normally attached to baby’s foot or hand. Sometimes babies have two sats probes on.
Respiratory support
Respiratory support helps to support baby’s breathing. There are many forms of respiratory support.
Forms of respiratory support
Intermittent Positive Pressure Ventilation (IPPV) using a Neopuff Infant T-Piece Resuscitator
- Nasal prong/low flow oxygen
- High flow nasal cannula (HFNC)
- Continuous Positive Airway Pressure (CPAP)
- Duo Bilevel Positive Airway Pressure (DuoPAP)/Bilevel Positive Airway Pressure (BiPAP) Ventilation
- Conventional Ventilation
- High Frequency Oscillatory Ventilation (HFOV)
- Inhaled nitric oxide (iNO)
The Neopuff/T-piece resuscitator is able to give breaths or pressure support to your baby by a mask or by their breathing tube if they have one. If your baby stops breathing, the nurses and doctors looking after them can use the Neopuff with a mask to re-start their breathing. The mask fits over your baby’s nose and mouth and gives the breaths into baby’s lungs.
This provides a small amount of extra oxygen into the air that your baby breathes in, which passes through two small tubes placed in a baby’s nose (nasal prongs). Normally at most 2 litres of extra oxygen per minute are given through the nasal prongs.
High flow nasal cannula can be used to give a mixture of warmed and moistened air and oxygen into baby’s nose. High flow gives a higher flow than low flow nasal prongs.
 Babies who need breathing support can find it very difficult to open up their lungs with each breath. Think of it like when you let the air out of a blown-up balloon, there will be a small amount left in the balloon making blowing it up again easier. The baby’s lung on CPAP is similar to the balloon, making breathing easier for them – the CPAP keeps the lungs open when baby breathes out. CPAP is given by a mask over baby’s nose or two little prongs into baby’s nose. CPAP can give a mixture of air and oxygen.
Babies who need breathing support can find it very difficult to open up their lungs with each breath. Think of it like when you let the air out of a blown-up balloon, there will be a small amount left in the balloon making blowing it up again easier. The baby’s lung on CPAP is similar to the balloon, making breathing easier for them – the CPAP keeps the lungs open when baby breathes out. CPAP is given by a mask over baby’s nose or two little prongs into baby’s nose. CPAP can give a mixture of air and oxygen.
DuoPAP/BiPAP gives CPAP at a higher and lower pressure.
 A ventilator is used to help babies to breathe. This machine gently pushes air through an ET tube (see ET Tube) down into baby’s lungs. The ventilator can tell if baby is trying to breath and is able to help the breaths that baby wants to take. The ventilator is also able to adjust itself if baby’s lungs are getting better. There are lots of things that the team looking after your baby can change on the ventilator to change how it helps baby’s breathing.
A ventilator is used to help babies to breathe. This machine gently pushes air through an ET tube (see ET Tube) down into baby’s lungs. The ventilator can tell if baby is trying to breath and is able to help the breaths that baby wants to take. The ventilator is also able to adjust itself if baby’s lungs are getting better. There are lots of things that the team looking after your baby can change on the ventilator to change how it helps baby’s breathing.
HFOV works in a different way than normal ventilation. It moves small amounts of air very quickly – it might look like your baby is vibrating. Babies who need HFOV often have very sick lungs. HFOV can be given by two different ventilators that look quite different.

iNO is a gas which is able to reduce the blood pressure in a baby’s lungs to let oxygen get from baby’s lungs into their blood. It is used to treat high blood pressure in the lungs (see PPHN). It is given through a machine that is attached to the ventilator or the CPAP/high flow machine.
Vital Signs Monitor
‘Vital signs’ is the term used for the markers that show how well a baby’s major body systems are working.
Vital signs
- Breathing rate: this is how fast baby breathes in a minute. A normal breathing rate in a baby can range from 30 to 60 breaths every minute, but some babies may breathe faster or slower than that.
- Heart rate: this is how often baby’s heart beats in a minute. A normal heart rate for a term baby ranges from 100 to 160 beats per minute, but some babies may have slower or faster heart rates.
- Blood pressure.
- Temperature.
- Oxygen saturation: this is the amount of oxygen in baby’s blood.
Babies in intensive care are attached to vital signs monitors all of the time. All babies on these monitors have oxygen saturation monitoring (see sats probes). Little stickers can be stuck on a baby’s chest to count their heart rate and breathing rate. Some babies have blood pressure sensors attached to their belly button, and other babies have little blood pressure cuffs. Babies’ monitors can alarm for lots of reasons, and only some of these reasons need us to go to baby immediately.